INTERPRETING your test results IN MORE DETAIL
Your COVID-19 Antibody Immunity Profile
Interpreting your Results – Carefully
Interpreting your results requires a degree of care and understanding. Your COVID-19 Antibody Immunity Profile contains 5 results that are all measured fully quantitatively and so, uniquely can be comparted. Unlike other platforms, the results allow us to understand in more details the mechanisms behind immunity.
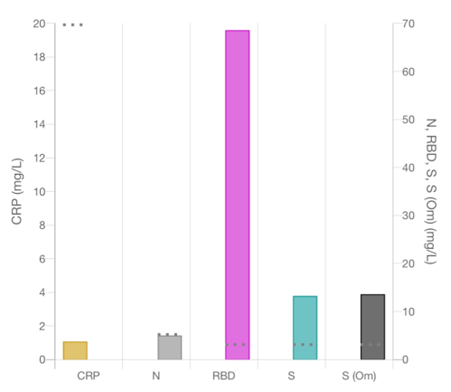
The profile consists of C reactive protein and antibody concentrations in your blood to Nucleocapsid (N), the Receptor Binding Domain (RBD), the Spike Protein (S) and the Omicron variant of the spike protein (SO). The answers are given in mg/L, a fully quantitative scientific measurement.
Your COVID-19 immunity comes from many events including, natural infection, vaccination with either a single jab and second jab, vaccinated and then boosted with all possible combinations of vaccines and then infections occurring symptomatically or asymptomatically between any of the vaccination or booster events. There is a very broad and different immunity profile in the community so there is no longer an ‘average’ – you need to know your own immunity profile.
C Reactive Protein (CRP) – a sensitive inflammatory marker
CRP is one of the most widely tested markers in the medicine and is very sensitive to any inflammation in the body. When you are healthy the normal levels are around 4-5 mg/L and up to 20 mg/L – the threshold for this test. If you have inflammation such as rheumatoid arthritis or an injury from the gym the CRP level may rise, and in the case of the gym injury fall again back to normal for you. If you have an infection such as COVID patients on admission to hospital have CRP levels around 40 – 60 mg/L and those who become really sick have CRP levels above 300 mg/L. Bacterial infections also trigger the CRP response and if your test results is above 20 mg/L we would expect your it to return to normal later, or you can explain it or perhaps need to mention it to a doctor.
Nucleocapsid (N) IgG Antibody Concentration
The N protein of the virus is inside and caries the mRNA but causes a large antibody response when you have significant infection. Patients in hospital have a very large N response when the condition has become systemic or viraemic. If you have had a bad infection previously, then your N antibody levels will be above the threshold which is set at 5.5 mg/L, the threshold level for patients from separating pre-pandemic and infections with the Wuhan variant in the first wave of the pandemic.
The variant is important and the new observation with the Omicron variant, especially amongst people who have been vaccinated or having a second infection, is that N does not always go above the threshold because the infection was not severe.
Receptor Binding Domain (RBD) IgG Antibody Concentration
The RBD is a region of the spike protein at the very tip and is responsible for docking with the cells of our body at the ACE2 receptor. The RBD antibodies are called neutralising antibodies because they neutralise the ACE2 receptor binding.
The neutralising antibodies are formed by either a natural infection or by the vaccine response, indeed some vaccines are optimised to make antibodies to this region of the spike protein. We often measure large concentrations of RBD in the blood over 150 mg/L and this is protective.
Neutralising antibodies levels above threshold are protective and the further above the longer you will have protection – but protection wanes.
Spike Protein IgG Antibody Concentration
The antibodies to spike include the neutralising antibodies for the tip as well as opsonising antibodies that offer protection by covering virus to prevent it entering the body. The S antibodies are produced in during infection and in response to the vaccines. The neutralising antibodies and covering antibodies work as part of the protection of infection in the nose.
Spike Omicron IgG Antibody Concentration
The spike protein has changed significantly from the Wuhan variant of SARS-CoV-2 and the Omicron variant is currently the most prevalent. It has 33 mutations that make it different from S and so the biding to SO is a measure of how well you will be protected against the current variant of concern.
If you have had the Omicron infection recently, you may have a higher SO concentration than S concentration. We are seeing this in some patients but not all as it depends on the how big the exposure to Omicron was.
Understanding More About Protection
Thresholds – Nasal Mucosa Antibody Protection from Infection
Attomarker has determined a unique threshold for immunity protection based on antibody levels in the nasal mucosa. Only because we know the concentration accurately of antibodies in the blood are we able to estimate the number of antibodies in the nose and hence determine the protective nasal threshold. We think this is a better way to manage the vaccine to personalise it to each patient and ensure that patient does not get an infection rather than get sick.
The threshold of 3.4 mg/L applies to S and SO and is derived from the vaccine response. Patients with two jabs from Pfizer or AZ were 93% and 67% less likely to develop infection. We measured the antibody levels for the two vaccine responses and determined the threshold based on the 93% and 67% efficacy to get the 3.4 mg/L. The prevention a getting infection was proven in more than 30,000 patients in the safety trials of the vaccines.
Lower levels of antibodies, below the threshold of 3.4 mg/L, will results in infection but not too badly and hopefully preventing the need to go to hospital. However, getting sick raises the risk of Long Covid.
Waning Immunity – Immunity Days and the ‘Edge of Immunity’
The antibody levels in the blood, and hence the nose, are not constant and they are falling with time. Antibodies halve their concentration in the blood every 60 – 200 days and that is a personal parameter called the half-life. If we take the shortest time at 60 days, then we can calculate how quickly your antibody levels will fall below the threshold. The shortest time that gives you the ‘edge of immunity’. The only way to be sure would be to take another test in 60 days’ time and see of the levels have fallen by a factor of 2.
So, your immunity days result shows you when you reach the edge of immunity and the risk of getting an infection begins to increase. Remember it depends on our antibody half-life however. It is a useful warning that things may begin to change and if you are eligible for a booster then this would be a good time to consider it. If you have had COVID since the measurement either symptomatically or asymptomatically then the edge of immunity will change.
Variants and Vaccine evasion
The vaccines were made to be protective against the Wuhan variant that started the pandemic in 2019 but we know that has changed through Alpha, Beta, Gamma, Delta and now Omicron variants. The vaccine efficacy varies from variant to variant: up to 50% of antibodies made to the initial vaccine do not binding to the spike Omicron protein. The poor binding means the threshold for Omicron could be higher, up to 6.4 mg/L and so we can calculate Omicron Immunity Days which may be shorter.
If the threshold for a particular variant becomes too high, above the levels of antibodies made by the vaccine close to the last booster, then there will be no protection from infection and the variant will be close to evading the vaccine. Greater numbers of infections will increase the chances of making variants that may evade the vaccine. We are seeing this already with Omicron BA.4 and BA.5 to new variants of concern according to ECDC.
Therefore keeping prevalence down now is highly desirable. As is having discretion over the administration of boosters. Smart boosting to boost those in the population and workforce currently at or below the edge of immunity will serve to protect those who are more vulnerable to infection than others who have significant levels of antibodies. Boosting this latter group is not only potentially unnecessary but brings with it attendant risks of avoidable auto-immune responses.
Personal Risk Management
Attomarker believes the Antibody Immunity Profile information is key to personal risk management and to maintaining business continuity
There are some caveats:
A huge viral load as a result of, say, a sneeze to the face, may overwhelm the nasal mucosa, and infection may occur. His quality masks partially mitigate this risk. The local prevalence is also likely to be a factor – increasing rates of daily exposure will again strain the immune defences.
T cells are obviously important. However, they are in low numbers in the nasal mucosa, where the ASRG believes, and there is significant literature to support, that antibodies covering the virus (oponisation) is the front line defence mechanism.